The term “rural healthcare” often evokes images of a singular doctor traveling between homesteads by horse and buggy. In reality, 97% of today’s U.S. geography — nearly a quarter of the U.S. population — falls under rural healthcare delivery. With the population spread out over a wide land area, the geography of rural America makes access to healthcare a prominent challenge.
While urban and rural healthcare centers worry about similar issues, this article will take a look at some of the main challenges facing rural healthcare: population, place, professionals, and pathways.
POPULATION
Pre-existing conditions are one of the most influential determinants to the community’s health. Rural populations tend to see a higher incidence of risk factors such as obesity, heart disease, diabetes, and addiction due to a lack of regular individualized healthcare — in fact, studies show that chronic health conditions tend to increase as rurality increases.
The culture behind a community also heavily impacts the health of its people. Rural communities have been found to be 1.7 times more likely to avoid healthcare visits than their
urban counterparts.
Rural culture is derived from generations of “self-care” — believing themselves to be “more hearty.”
Privacy is also a challenge in rural communities as many patients are familiar with the doctors, nurses, and other patients in the healthcare setting. This is most commonly seen in the area of mental health. Rural residents are less likely to participate in their healthcare system for two reasons: the perceived “neighbor” stigma, and the lack of coordination of healthcare resources.
PLACE
Rural populations often require travel for healthcare services, and, as a result, are looking for a one-stop-shop approach when they arrive. Patients do not want to go to three different providers in three different parts of town. Ideally, they need a campus or a clinic with an integrated model of care where they can easily navigate between all appointments in a single day.
Hospitals can be frightening for many people who don’t want to go to a sterile medical setting for outpatient services. There is also a current push for decentralized community care to reduce the number of steps between appointments. Outpatient services are gravitating away from the hospital and into smaller, freestanding medical office buildings that include amenities such as retail, a coffee shop, and fitness.
For rural healthcare centers that don’t have the luxury of a multiple-building campus or access to a wide variety of providers, “neighborhoods” within a single building provide individualized outpatient services without the hospital feel.
PROFESSIONALS
The greatest challenge for rural communities is access to healthcare staff. According to the American Hospital Association, two-thirds of the nation’s Health Professional Shortage areas are located within rural areas.
Rural healthcare systems face two issues related to staffing: not enough money to bring on more staff, and not enough staff interested in working for their systems. Healthcare is already following a trend of ultra-specialization by providers. This has resulted in fewer general practitioners, and also a heightened expectation of doctor specialization by patients.
PATHWAYS
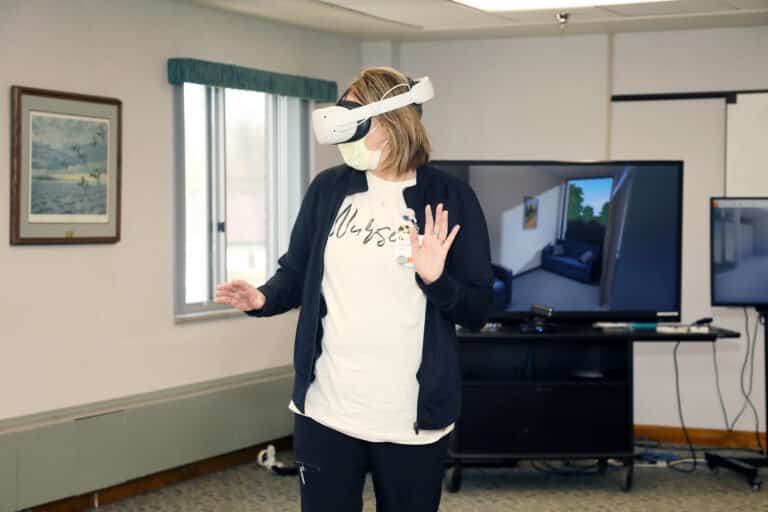
Technology such as telehealth, wearables, and virtual hospitaling are game changers for futureproofing rural healthcare. In the past, rural hospitals sent patients out of the community for hospital-based or specialty services. The pandemic has helped fast-track the ability to connect patients and providers for a “close to home” healthcare experience. For example, a patient now may have one in-person visit, followed by two telehealth checkups using at-home equipment such as a blood pressure cuff or an oxygen monitor.
Telehealth connects patients to the care they need, and also provides a collaboration tool for providers. In an area with scarce healthcare resources, collaboration between providers is essential for promoting population health. As high speed internet access in rural communities improves, telehealth will provide better access to care.
WHAT’S NEXT?
Architects and designers have a growing responsibility in addressing healthcare delivery, research, and equity. With post-pandemic rural communities in a state of change, one of the most important pieces is to start looking at the data from the pandemic. Rural communities are going to be different, both qualitatively and quantitatively. Unfortunately, the quantitative data that is currently available is extremely outdated.
Therefore, the first crucial step is to work to create new methods of collecting data to help better advocate for the needs of the community.
Redefining the role of the design professional to think “Beyond the Building” will be increasingly valuable. Firms need to serve clients outside of the brick and mortar and start setting the stage as strategic partners; partners who look at building great community connections. A strong emphasis will also need to be placed on dignity, equity, and the positive impact of design to uplift humanity.
Design is a force for change. Earlier involvement for architects, designers, and community members in the design process will lead to earlier concepts, ideas, solutions, and master plans. When design professionals are engaged at the forefront, it will allow them to gather initial community thoughts and use their expertise to lead to a well-rounded solution. This involvement should not end after project completion, but rather continue throughout post-occupancy evaluations to address improvements and future positive change.
When it comes to defining strategies for improving rural healthcare, now is the time. We have new technology to build upon design excellence, delivering opportunities in population health, wellness, and research.